Can a Plant-Based Diet Help Reverse Type 2 Diabetes?
Key takeaways
- Type 2 diabetes remission is possible through dietary changes without surgery or medication.
- A whole-food, plant-based diet supports better blood sugar control and insulin sensitivity.
- Clinical experts now recognize lifestyle and diet as frontline interventions for diabetes.
- Real-world studies show significant medication reduction and remission using plant-predominant diets.
- Keto and low-carb diets may offer short-term gains but come with potential long-term health risks.

The Rising Cost and Human Toll of Type 2 Diabetes
Type 2 diabetes isn’t just a personal health concern — it’s a public health crisis. Every year, roughly 1.5 million people die from complications tied directly to diabetes. What’s more alarming is that the majority of these cases could have been prevented, and in many situations, managed without spiraling into life-altering complications like kidney failure, stroke, heart attacks, or amputations.Rethinking the Standard Treatment Model
For decades, diabetes management has revolved around one thing: controlling blood sugar with medication. While drugs like metformin or insulin can stabilize glucose levels, they rarely address the deeper issue — insulin resistance driven by lifestyle and dietary patterns. More often than not, the focus remains on symptom control, not resolution.What Remission Really Means in Type 2 Diabetes
The word “remission” used to be reserved for conditions like cancer. But today, there’s a growing consensus that type 2 diabetes — often deemed “chronic and progressive” — doesn’t have to be a lifelong sentence.According to a panel of medical experts from organizations such as the American College of Lifestyle Medicine, the American Heart Association, and the Academy of Nutrition and Dietetics, type 2 diabetes remission should be defined as maintaining HbA1c levels below 6.5% for at least three months without the use of medications, devices, or surgery. And diet — not drugs — was cited as the most powerful lever to achieve this.
How a Plant-Based Diet Impacts Blood Sugar Control
Plant-based diets rich in fiber, legumes, vegetables, whole grains, fruits, and seeds have been shown to directly impact insulin sensitivity. Fiber slows glucose absorption, reduces blood sugar spikes, and feeds beneficial gut bacteria — which in turn can improve metabolism.Clinical Endorsements: Shifting Toward Food as Medicine
What’s groundbreaking isn’t just that plant-based diets work — it’s who’s now backing them. Medical consensus is gaining traction, not just among fringe groups or niche wellness circles, but from credentialed bodies like the American College of Cardiology and the Academy of Nutrition and Dietetics.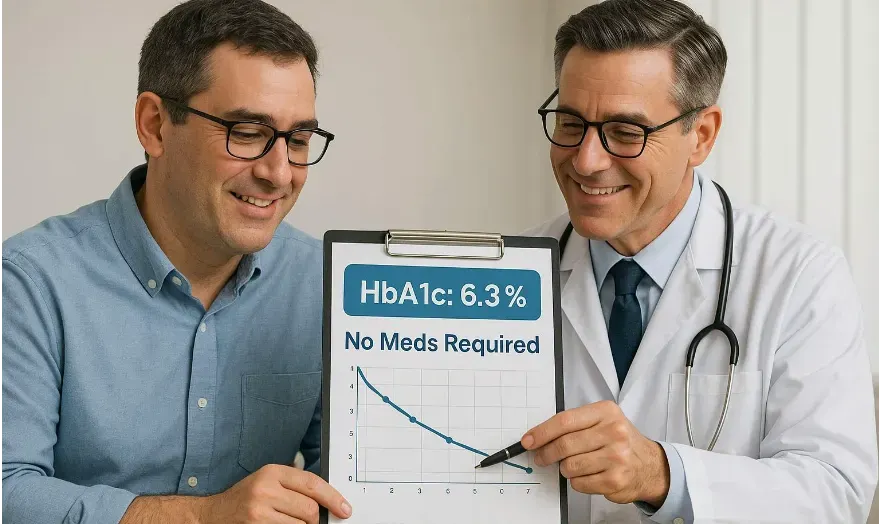
In an official consensus statement, remission was promoted not as an aspirational goal but as a clinical one — achievable primarily through a whole-food, plant-predominant diet. That marks a pivotal moment in diabetes care, shifting nutrition from an afterthought to a frontline strategy.
The Real-World Impact: Study Findings on Diet-Driven Remission
In one real-world application, patients were referred to a wellness clinic and advised — as part of their routine medical care — to adopt a high-fiber, plant-predominant diet without drastic caloric restriction. This wasn’t a tightly controlled research study with hand-picked participants. These were regular people, simply offered education and support.Debunking Low-Carb Myths in Diabetes Management
There’s been a lot of noise around low-carb and ketogenic diets as solutions for diabetes. While they can produce short-term blood glucose improvements, they often come with trade-offs: increased LDL cholesterol, poor long-term adherence, and reduced nutrient diversity.In contrast, plant-based diets have shown positive cardiometabolic effects — improving cholesterol, blood pressure, and inflammation. The goal shouldn’t be a temporary glucose fix, but lasting metabolic health. And that means favoring interventions that support the heart, brain, kidneys, and gut — not just the glucose meter.
Practical Steps: What a Plant-Predominant Diet Looks Like
So, what does this way of eating actually look like day-to-day? Think of your plate as 95% plant-sourced. Fill it with:- Legumes like black beans, lentils, and chickpeas
- Whole grains such as oats, brown rice, quinoa
- Fruits and vegetables — aim for color and variety
- Nuts and seeds in moderation for healthy fats
Beyond Remission: Long-Term Benefits and Lifestyle Gains
Even if remission isn’t reached immediately, adopting a plant-forward eating style pays off. People often experience more energy, better digestion, weight loss, improved mood, and a reduced need for medications across the board — not just for diabetes, but also for blood pressure, cholesterol, and joint health.Final Thoughts: Food, Freedom, and the Future of Diabetes Care
What we eat has the power to transform how we live. The evidence is stacking up: a plant-predominant diet isn’t just a health trend — it’s a therapeutic tool. One that doesn’t just manage type 2 diabetes, but in many cases, sends it into remission. More importantly, it offers something medication alone can’t: autonomy. When people learn how to nourish themselves differently, they gain more than glycemic control — they gain freedom. And that’s the kind of healthcare we should all be working toward.References:
- Del Carmen Fernández-Fígares Jiménez M. Plant foods, healthy plant-based diets, and type 2 diabetes: a review of the evidence. Nutr Rev. 2024;82(7):929-948.
- Biener AI, Decker SL, Rohde F. Source of increased health care spending in the United States. JAMA. 2019;321(12):1147.
- Schlesinger S. Diet and diabetes prevention: is a plant-based diet the solution? Diabetes Care. 2023;46(1):6-8.
- Rosenfeld RM, Kelly JH, Agarwal M, et al. Dietary interventions to treat type 2 diabetes in adults with a goal of remission: an expert consensus statement from the american college of lifestyle medicine. Am J Lifestyle Med. 2022;16(3):342-362.
