How the Ketogenic Diet Boosts Brain Health: From Mitochondria to Mental Wellness
A New Lens on Brain Health Through Ketogenic Nutrition
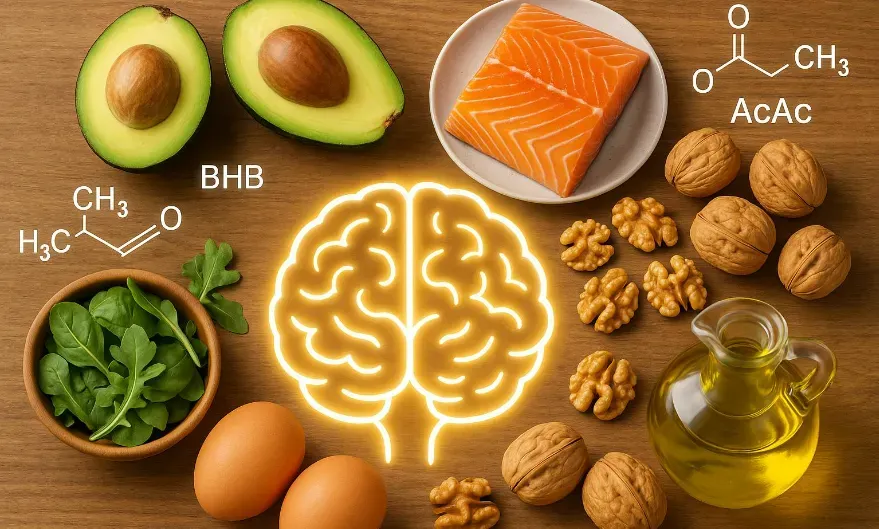
There’s growing intrigue around how a high-fat, low-carbohydrate ketogenic diet impacts the brain—and not just for epilepsy anymore. What started as a clinical intervention for seizure disorders is now showing serious promise for psychiatric conditions like schizophrenia, bipolar disorder, and major depression. At the core of this metabolic therapy lies its influence on mitochondria—the microscopic power plants in our cells—and the cascade of effects they drive in brain function.
The ketogenic diet mimics the fasting state, shifting the body from using glucose to using ketones for fuel. This shift initiates a wave of cellular changes, particularly in brain cells where energy supply is everything. When glucose availability dips, neurons are nudged into a more efficient, resilient metabolic mode. This has consequences not just for seizure control, but also for mood regulation, cognition, and even long-term neuroprotection.
The Mitochondrial Mechanism Behind Ketogenic Benefits
Mitochondria don’t just churn out energy—they're gatekeepers of cell survival, signaling, and renewal. What the ketogenic diet appears to do is rev up mitochondrial function in a way that’s hard to achieve through other means. Preclinical studies show ketogenic diets enhance mitophagy (clearing out damaged mitochondria) and stimulate mitochondrial biogenesis—essentially making way for newer, healthier mitochondria.
This cellular cleanup boosts the efficiency of energy production, crucial for neurons, which are especially vulnerable to mitochondrial dysfunction. Some of the most compelling findings come from animal studies where ketogenic interventions led to genetic changes centered on mitochondrial pathways. These changes have been directly tied to reduced seizure activity and improvements in cognitive performance.
Psychiatric Disorders and the Role of Brain Energy Metabolism
Mental health disorders like schizophrenia and bipolar disorder aren’t just psychological—they have biological roots, especially in how the brain handles energy. Traditional psychiatric meds often focus on neurotransmitter modulation, but what if the problem lies deeper—in the metabolism of the brain itself?
Pilot studies and case reports involving over 1,900 individuals indicate that the ketogenic diet can induce remission in some people with treatment-resistant mental illness. In one UK trial, bipolar patients saw not only physical health improvements like better blood pressure and weight management but also a measurable reduction in brain hyperactivity—likely linked to excess glutamate, a key neurotransmitter involved in excitability.
Gut-Brain Axis: A Surprising Player in Neurological Health
Another layer of the story lies in the gut. Researchers have discovered that changes in gut microbiota from ketogenic diets can affect brain function—without even altering the brain directly. In one striking study, fecal samples from children on a ketogenic diet transferred to epileptic mice reduced the mice's seizures. That suggests something in the gut—possibly microbes, neurotransmitters, or peptides—is communicating with the brain.
And it's not an either-or equation. The gut microbiome and mitochondrial function are both in play, likely working together in a complex dance of signaling pathways. What begins in the digestive tract may culminate in changes to how mitochondria operate in the brain—fueling the idea that brain disorders can stem from metabolic and microbiome disruptions.
Is Ketosis a Tool for Everyone—or Just for the Sick?
The science supporting ketogenic diets in clinical populations is compelling. But what about healthy individuals? Could cycling in and out of ketosis, or incorporating intermittent fasting, provide cognitive or metabolic advantages? According to emerging data, the answer leans toward yes.
Ketogenic strategies may serve as a preventive tool by enhancing mitochondrial efficiency and reducing inflammation—even in those without diagnosable conditions. While the research isn’t as extensive due to limited funding, the parallels to fasting, a practice embedded in human tradition, offer some reassurance. From ancient rituals to modern biohacks, fasting and ketosis have long histories of use for clarity, healing, and renewal.
Nutritional Precision and Cautions for Ketogenic Practices
Before jumping headfirst into ketosis, nuance matters. Like fasting, ketogenic diets aren't universally safe or beneficial unless done correctly. The extreme version of fasting is starvation—which is obviously harmful. Similarly, a poorly constructed ketogenic plan can lead to nutrient deficiencies or excessive intake of unhealthy fats.
Ensuring adequate intake of calories, vitamins, minerals, and hydration is non-negotiable. And if you’re exploring ketogenic strategies for mental health or chronic conditions, it’s worth doing so under medical guidance. Just as you wouldn't casually tinker with your medication dosage, shifting your brain’s energy metabolism demands respect and structure.
