How to Manage Irritable Bowel Syndrome: Effective Strategies and Insights

Irritable Bowel Syndrome (IBS) is a complex and often misunderstood condition that affects the gastrointestinal tract. Characterized by a combination of symptoms like bloating, diarrhea, constipation, and abdominal discomfort, IBS can significantly impact the quality of life of those affected. This article explores the multiple facets of IBS, delving into its causes, the intricate relationship between the gut and the brain, diagnostic approaches, and effective management strategies to provide relief and improve wellbeing.
What is Irritable Bowel Syndrome?
IBS is more than just an inconvenient set of gastrointestinal symptoms; it's a functional disorder meaning the symptoms are related to problems with how the gut works, though the exact cause remains elusive. Typically, it manifests through a variety of symptoms including but not limited to abdominal pain, bloating, and changes in bowel habits. This variability in symptoms often makes diagnosis and management a challenging endeavor, requiring a nuanced understanding of its mechanisms and triggers.
Common Symptoms and Diagnostic Challenges
Patients with IBS often report a diverse range of symptoms, which can include severe bloating, constipation, and diarrhea. These symptoms can fluctuate over time, complicating the diagnostic process. Traditionally, IBS is diagnosed based on clinical criteria after ruling out other inflammatory or structural abnormalities of the gut through diagnostic tests like colonoscopies and blood tests. This process underscores the need for precise and careful assessment to ensure accurate diagnosis and appropriate treatment planning.
Key symptoms of IBS include:
- Abdominal pain and cramping that often decrease after bowel movements
- Altered bowel habits (constipation, diarrhea, or both)
- Bloating and gas
- Food intolerance which can exacerbate symptoms
Understanding these symptoms and their impacts can significantly aid in navigating IBS management.
The Gut-Brain Connection in IBS
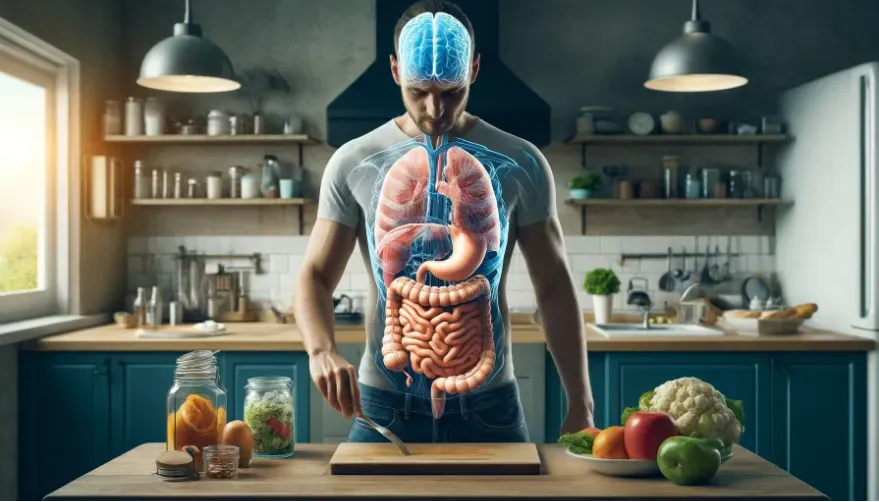
IBS is closely linked to the gut-brain axis, a complex communication network involving nervous and hormonal messages. This axis plays a pivotal role in ensuring gut function and managing physical and psychological stress which can affect gut health. Understanding this connection helps in comprehensively addressing the root causes of IBS symptoms and improving patient outcomes.
How Gut Motility Influences IBS
Gut motility—the movement of the digestive system that helps the body digest and move food—can be either too slow or too fast in IBS patients, leading to constipation or diarrhea respectively. Disruptions in the normal motility patterns can significantly contribute to the typical symptoms of IBS. Treatments often aim to normalize this motility, using dietary changes, medications, and sometimes psychological interventions to manage stress and anxiety, which are closely linked to gut motility.
Impact of Stress and Mental Health on IBS
Stress and mental health play critical roles in the onset and exacerbation of IBS symptoms. Stress can directly affect the gut-brain communication, leading to altered gut motility and sensitivity. Managing stress through techniques such as mindfulness meditation, regular exercise, and adequate sleep can significantly mitigate these effects and improve symptoms.
Effective stress-reduction techniques include:
- Mindfulness meditation: Focuses on being intensely aware of what you're sensing and feeling at every moment.
- Regular physical activity: Such as walking, yoga, or swimming that can help reduce the overall stress levels.
- Adequate sleep: Ensuring 7-9 hours of quality sleep per night helps reduce stress and improve gut health.
Key Causes and Triggers of IBS
Identifying the underlying causes and triggers of IBS is essential for effective management. While the exact cause is unknown, factors such as genetics, prior gastrointestinal infections, and chronic stress are known contributors. Additionally, food sensitivities and allergies can trigger symptoms and managing these through dietary adjustments can be a crucial aspect of treatment.
Post-Infectious IBS: Understanding the Long-term Effects
Post-infectious IBS occurs after a significant gastrointestinal infection, such as food poisoning. This type can persist long after the initial infection has resolved, as the immune system continues to react, potentially leading to chronic inflammation and altered gut function. Understanding this mechanism highlights the importance of managing gut health post-infection to prevent the progression to chronic IBS.
SIBO and Its Role in Exacerbating IBS
Small Intestinal Bacterial Overgrowth (SIBO) occurs when there is an abnormal increase in the population of bacteria in the small intestine. This overgrowth is linked to many cases of IBS, particularly those involving predominant bloating and diarrhea. Managing SIBO through antibiotics, dietary changes, and probiotics can significantly relieve IBS symptoms.
Diagnostic Tests for IBS and Related Conditions
Accurate diagnosis of IBS involves a comprehensive approach that includes ruling out other conditions that mimic its symptoms. This is typically achieved through a combination of symptom assessment, blood tests, and sometimes more specialized tests like stool samples or breath tests for detecting SIBO.
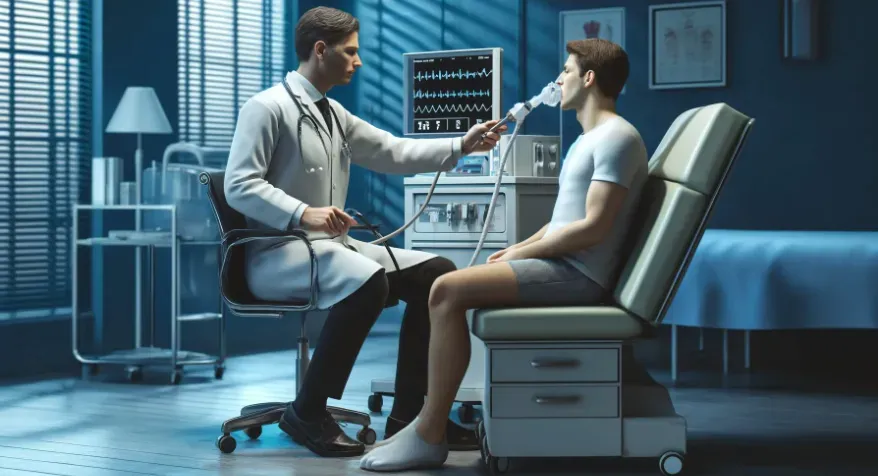
The Role of the IBS Smart Test
The IBS Smart Test is a relatively recent development that checks for specific antibodies often elevated in post-infectious IBS. This test can be a valuable tool in identifying this subset of IBS patients, allowing for targeted treatment strategies that address the unique aspects of their condition.
Testing for SIBO: Methods and Importance
The lactulose breath test is the primary diagnostic tool for detecting SIBO. It measures the levels of hydrogen and methane that are byproducts of bacterial metabolism in the gut. Elevated levels suggest an overgrowth of bacteria, confirming the presence of SIBO and facilitating targeted treatments that can alleviate related IBS symptoms.
Effective Treatments and Management Strategies for IBS
Managing IBS effectively requires a multifaceted approach tailored to the individual's specific symptoms and underlying triggers. This includes dietary modifications, pharmacological treatments, and lifestyle changes aimed at reducing stress and improving overall gut function.

Diet and Lifestyle Adjustments for IBS Relief
The Low FODMAP diet is frequently recommended for IBS management. This diet involves limiting foods that are high in fermentable oligosaccharides, disaccharides, monosaccharides, and polyols, which can exacerbate symptoms like bloating and gas. Besides dietary changes, lifestyle adjustments such as increased physical activity and regular eating schedules can also help manage symptoms.
Supplements and Natural Remedies for IBS
Supplements such as peppermint oil, ginger, and probiotics are commonly used to manage IBS symptoms. These natural remedies can help soothe the gut, reduce bloating, and improve overall digestive health. It’s crucial, however, to consult healthcare professionals before starting any new supplement regimen.
Prescription Medications and Their Applications
For some individuals, prescription medications may be necessary to manage severe or persistent IBS symptoms. Medications like antispasmodics, laxatives, and SSRIs are used depending on whether the predominant symptoms are pain, constipation, or diarrhea. Emerging treatments like prokinetics also offer new hope by improving gut motility.
The Role of Lifestyle in Managing IBS Symptoms
Lifestyle plays an undeniable role in both the development and management of IBS. Regular physical activity, adequate hydration, and a balanced diet can profoundly impact gut health and symptom severity.

The Importance of Physical Activity
Physical activity, particularly low-impact exercises like walking or yoga, can improve gut motility and reduce stress levels, both of which are beneficial for IBS sufferers. Integrating regular movement into daily routines is a simple yet effective strategy for managing IBS symptoms.
Stress Reduction Techniques and Their Benefits
Stress management is pivotal in controlling IBS. Techniques such as deep breathing exercises, yoga, and mindfulness meditation can help reduce the physiological stress responses that exacerbate IBS symptoms. Regular practice of these techniques can help establish a more relaxed and balanced gut environment.
Conclusion: Integrating Knowledge for Effective IBS Management
In conclusion, IBS is a multifaceted condition that requires a comprehensive and personalized approach for effective management. By understanding the various components—from gut-brain interactions to the impact of diet and lifestyle—patients can work towards controlling their symptoms and enhancing their quality of life. Collaboration with healthcare providers, commitment to self-care, and ongoing education are crucial in navigating the challenges of IBS.
