Unlock the Keys to Managing Hypertension and Reducing Cardiovascular Risk
Understanding Hypertension and Cardiovascular Risk
What is Hypertension?
Definition and Causes
Hypertension, often referred to as high blood pressure, is a condition in which the force of blood against artery walls is too high, persistently. This condition can be triggered by various factors including genetics, poor diet, lack of physical activity, and excessive salt intake. Over time, elevated pressure can cause wear and tear on the arterial walls, leading to various health problems.
Primary contributing factors to hypertension include:
- Genetics: A family history of hypertension can increase one's risk.
- Dietary choices: High salt intake, high fat, and low potassium intake can elevate blood pressure.
- Physical inactivity: Lack of regular exercise contributes to weight gain, which is a strong risk factor for hypertension.
Blood Pressure Readings
Blood pressure is measured using two numbers: systolic and diastolic. Systolic pressure represents the pressure when the heart beats, while diastolic pressure stands for the pressure when the heart is resting between beats. A normal reading would be under 120/80 mmHg. Readings consistently above 130/80 mmHg are generally considered in the hypertension range.
Understanding Blood Pressure Categories:
- Normal: Less than 120/80 mmHg
- Elevated: 120-129/less than 80 mmHg
- Hypertension Stage 1: 130-139/80-89 mmHg
- Hypertension Stage 2: 140 or higher/90 or higher
Prevalence of Hypertension
Approximately half of the adults in the U.S. over the age of 20 are affected by hypertension, with a lifetime risk nearing 90%. This widespread prevalence underscores the critical need for effective management strategies and a deeper public understanding of the condition.
What is Cardiovascular Risk?
Key Risk Factors
Cardiovascular risk refers to the potential of a person to develop heart conditions due to existing factors. Key risk factors include hypertension, smoking, high cholesterol, diabetes, obesity, and a family history of heart disease. These factors can significantly increase the risk of developing heart-related illnesses.
Global Risk Assessment in Hypertensive Patients
Incorporating a global cardiovascular risk assessment for individuals with hypertension can significantly improve the outcome by customizing treatment strategies. This comprehensive assessment evaluates the combined risk posed by multiple factors, rather than focusing on hypertension alone. It helps to identify patients who might benefit from aggressive treatment approaches aimed at multiple risk factors.
Elements typically assessed in global risk evaluations include:
- Blood pressure levels
- Cholesterol levels
- Lifestyle factors such as smoking and diet
- Presence of diabetes
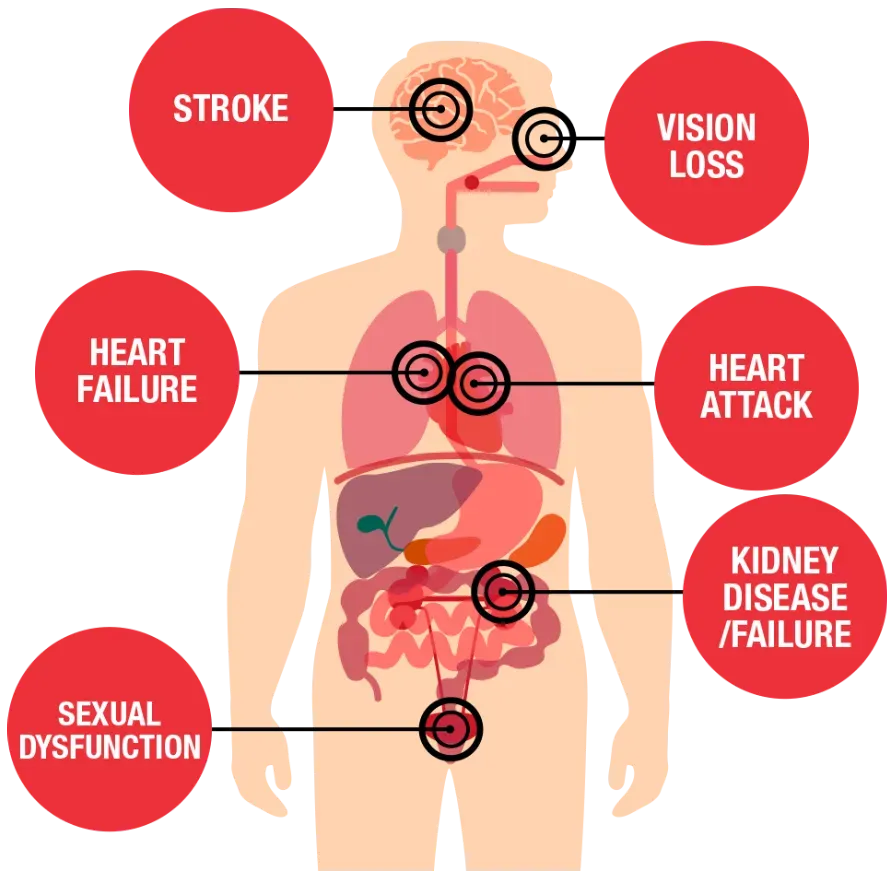
Health Impacts of Hypertension on Cardiovascular Systems
Effects of High Blood Pressure on the Heart
Heart Failure
Chronic hypertension can lead to heart failure, a serious condition where the heart cannot pump enough blood to meet the body’s needs. The increased workload from high blood pressure can cause the heart to enlarge and fail to supply blood efficiently.
Coronary Artery Disease
High blood pressure can cause coronary artery disease by accelerating atherosclerosis, which narrows and hardens the arteries leading to the heart. This can ultimately lead to chest pain, heart attacks, and other severe heart conditions.
Left Ventricular Hypertrophy
Hypertension forces the heart to work harder to pump blood, which can cause the left ventricle to thicken or stiffen (left ventricular hypertrophy). This alteration can impair the heart's ability to pump blood and might escalate the risk of heart failure, arrhythmia, and sudden cardiac death.
Effects on Blood Vessels and Organs
Stroke and Transient Ischemic Attacks
High blood pressure is the leading risk factor for strokes and transient ischemic attacks (TIAs). It can cause blood vessels in the brain to clog more easily or even burst, leading to a stroke.
Peripheral Arterial Disease
Hypertension can narrow and block the arteries that supply blood to the legs and arms, a condition known as peripheral arterial disease. This can result in pain, changes in skin color, sores, and difficulty in walking.
Retinal and Renal Damage
Persistent high blood pressure can also damage the delicate blood vessels that supply blood to the eyes and kidneys, leading to conditions such as retinopathy and kidney disease. These conditions can cause significant visual and renal impairments if not managed properly.
Detecting and Diagnosing Hypertension and Cardiovascular Risk
Blood Pressure Monitoring Methods
Home vs. Office Blood Pressure Readings
Monitoring blood pressure at home versus in a clinical setting can sometimes yield different results. Home monitoring can help identify 'masked hypertension'—where individuals have normal blood pressure readings in a clinical setting but elevated levels at home— affecting over 21% of men and 11% of women.
Ambulatory Monitoring for Temporal Patterns
Ambulatory blood pressure monitoring involves wearing a portable device that takes blood pressure readings at regular intervals over 24 hours. This method provides valuable insights into how blood pressure changes throughout the day and night, helping to identify hypertension and assess cardiovascular risk more accurately.
Diagnostic Testing
Blood Tests and Biomarkers
Routine blood tests can check for high cholesterol, kidney function, and other biomarkers that indicate cardiovascular risk. These tests are crucial for diagnosing and formulating a treatment plan for hypertension.
Electrocardiogram and Echocardiogram
An electrocardiogram (ECG) measures the heart's electrical activity and can detect irregularities, while an echocardiogram uses ultrasound to assess heart muscle and valve function. Both are vital in assessing the heart's health and determining the impact of high blood pressure on the cardiovascular system.
Coronary Artery Calcium Scans
This specialized scan uses computed tomography (CT) to detect calcification in the coronary arteries, an indicator of atherosclerosis. A higher calcium score might suggest a higher risk of myocardial infarction and other coronary events, particularly in people with hypertension.
Managing Hypertension to Lower Cardiovascular Risk
Lifestyle Interventions
Diet and Exercise
A heart-healthy diet—low in salt, saturated fats, and cholesterol, and rich in fruits, vegetables, whole grains, and lean protein—can significantly reduce blood pressure. Regular physical activity can also strengthen the heart muscle, improve blood flow, and lower blood pressure.
Weight Management and Smoking Cessation
Maintaining a healthy weight reduces the strain on the heart, while quitting smoking can significantly decrease the risk of heart disease. Both are crucial steps in managing hypertension and reducing overall cardiovascular risk.
Managing Stress and Alcohol Consumption
Stress and excessive alcohol intake can elevate blood pressure. Effective stress management techniques, such as meditation, regular exercise, and adequate sleep, along with moderated alcohol consumption, can help in maintaining optimal blood pressure levels.
Medical Treatments
Blood Pressure Medication Types
Several types of blood pressure medications, such as ACE inhibitors, beta-blockers, diuretics, and calcium channel blockers, can be used to manage hypertension effectively. The choice of medication often depends on the overall health profile and the specific needs of the individual.
Personalized Treatment Plans
Personalized treatment plans that consider all aspects of an individual's health can optimize hypertension management. This includes combining medications, lifestyle adjustments, and regular monitoring to tailor the approach for the best outcomes.
Future Directions in Hypertension and Cardiovascular Research
New Technologies for Blood Pressure Monitoring
Innovations in wearable technology and mobile health apps are making it easier and more efficient to monitor blood pressure continuously. These technologies promise to provide more precise and real-time assessments of blood pressure, allowing for better management of hypertension.
Innovations in Risk Assessment Tools
Emerging tools that incorporate artificial intelligence and machine learning are being developed to predict cardiovascular risk more accurately. These advancements could revolutionize how we assess and manage hypertension in the future.
Personalized Medicine Approaches
The field of genetics is providing insights into how individual genetic profiles can influence response to hypertension treatments. This could lead to more personalized, effective therapeutic strategies that consider genetic factors in the management of high blood pressure and cardiovascular risk.
Conclusion
Importance of Early Detection and Management
Early detection and effective management of hypertension are crucial in preventing serious cardiovascular events and other health complications. Regular monitoring and timely interventions can markedly reduce the risk and improve quality of life.
Primordial Prevention and Comprehensive Healthcare
Adopting a comprehensive approach that includes primordial prevention—avoiding the development of risk factors in the first place—is essential. This broad strategy, combined with personalized medical care, holds the potential for significantly better health outcomes for individuals at risk of or living with hypertension.