Understanding Cancer: How Cells Become Cancerous and Why Metastatic Cancer Is So Deadly
Key takeaways
- Cancer arises when genetic mutations cause uncontrolled growth and the ability to spread.
- Epithelial cancers account for about 90% of all cancer deaths due to their tendency to metastasize.
- Localized cancers are often curable; metastatic cancers rarely are.
- Only a few cancers—like germ cell, choriocarcinoma, melanoma, and renal cancer—can be cured after spreading.
- Preventing mutation accumulation and detecting cancers early remain our best defense.
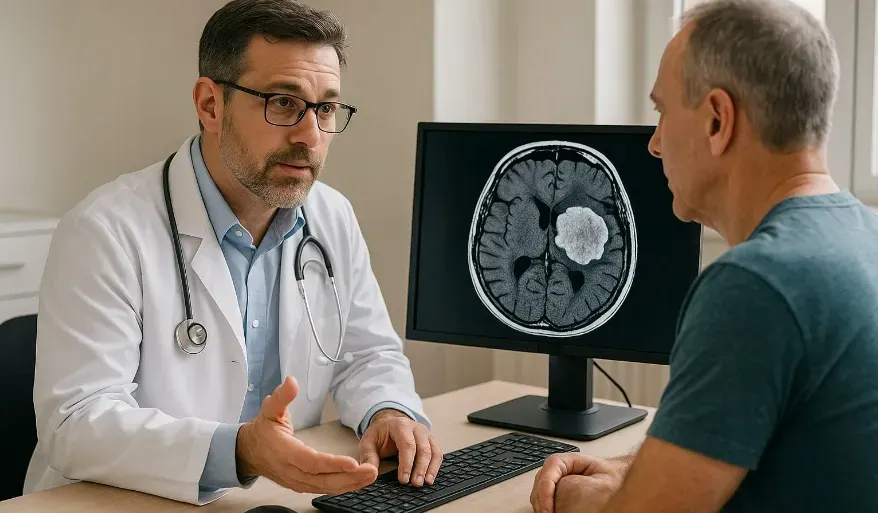
Cancer begins quietly—often with a single cell that refuses to follow the body’s normal rules. Over time, that lone rebel grows into a colony, then a mass, and in some cases, a disease capable of spreading throughout the body. Despite major breakthroughs in treatment and survival rates for certain cancers, metastatic cancer—when cancer spreads beyond its original site—remains the leading cause of cancer-related death worldwide.
What Makes a Cell Cancerous?
Uncontrolled Growth and the Loss of Normal Regulation
Normal cells in the body grow, divide, and die according to highly regulated instructions. Each tissue—whether skin, liver, or lung—knows when to stop growing. Cancer cells, however, lose that internal governor. They keep dividing even when they’re not supposed to, forming clusters or tumors that push aside healthy tissue.The Power to Invade and Spread
The second defining trait of cancer is its ability to metastasize—to break away from its original site, travel through the bloodstream or lymphatic system, and colonize distant organs. No normal cell in the body can do this. Cancer cells develop unique properties that allow them to detach, survive hostile environments, and re-establish growth elsewhere.
The Two Major Types of Cancer
Epithelial vs. Hematologic Cancers
Most cancers fall into two broad categories: epithelial and hematologic.
- Epithelial cancers, which arise from the cells lining organs and ducts, make up roughly 90% of all cancer deaths. These include cancers of the colon, breast, pancreas, lungs, prostate, and ovaries.
- Hematologic cancers, like leukemia and lymphoma, originate in the blood or bone marrow and represent the remaining 10%.
Why Epithelial Tumors Are So Common
The cells that line ducts in solid organs—such as the colon, lungs, or pancreas—turn over rapidly. Each new cell division carries a small risk of DNA error. Over decades, those errors add up. That’s why cancers of epithelial tissues are far more prevalent than those of the blood, muscle, or bone. The body’s regenerative power, ironically, becomes its vulnerability.From Local Tumor to Metastasis
The Turning Point
When a cancer remains local, confined to its tissue of origin, surgery can often remove it completely. For many solid tumors, more than half of patients diagnosed at this stage are cured and go on to live normal lifespans. But once the cancer spreads beyond the reach of a scalpel—into the bloodstream, lymph nodes, or distant organs—the odds change dramatically.Why Metastatic Cancer Is So Lethal
A tumor that has spread is no longer one disease; it’s many. Cancer cells that metastasize often evolve as they migrate, picking up new mutations and resistances along the way. A lung tumor that spreads to the brain, for example, behaves differently from the original lesion. This biological diversity makes systemic treatment extraordinarily difficult.Even with advanced chemotherapy or immunotherapy, complete and lasting remissions in metastatic solid tumors are exceedingly rare. For most, treatment aims to extend life and improve quality, not to cure.
Rare Exceptions: When Metastatic Cancer Can Be Cured
There are a few remarkable outliers. Certain germ cell tumors (like testicular cancer) and choriocarcinomas (cancers originating in placental tissue) respond so dramatically to chemotherapy that even extensive metastases can vanish completely. Similarly, melanoma and renal cell carcinoma have shown curative responses to immune-based therapies such as interleukin-2.
These exceptions prove that metastases can be reversed—but also highlight how limited our understanding remains. The vast majority of metastatic cancers—breast, colon, pancreatic, and lung—still resist every therapy we’ve developed to date.
Why Mutation Accumulation Drives Cancer Formation
The Role of DNA Damage and Repair
Every time a cell divides, it copies its DNA—a process involving billions of base pairs. Even with sophisticated proofreading, errors occur. Environmental insults like UV light, toxins, or chronic inflammation accelerate this process. Over years, a critical mass of mutations can disable tumor-suppressor genes (like p53) or activate oncogenes that drive growth.
Chronic Tissue Renewal: The Hidden Risk
Organs with high cellular turnover—like the colon, skin, or lungs—are especially susceptible. In these tissues, stem cells are constantly dividing to replace old cells. Every division introduces a small chance for error. It’s a numbers game that, over decades, tips in cancer’s favor unless balanced by DNA repair, immune surveillance, and lifestyle factors that minimize damage.The Urgent Need for Better Therapies
A Sobering Reality
Despite enormous progress in cancer research, metastatic solid cancers remain nearly universally fatal. For localized tumors, surgery and early detection save lives. But once cancer escapes its original site, no existing systemic therapy can reliably cure it—outside the rare exceptions mentioned earlier.
