Glutamine for Gut Health: A Neuroscience-Informed Strategy to Repair Your Gut Without Probiotics
Key takeaways
- Glutamine is essential for gut lining repair and supports immune and mood balance.
- Exercise, surgery, and chronic stress deplete glutamine and contribute to gut dysfunction.
- Magnesium and B6 are vital cofactors for converting glutamine into calming neurotransmitters.
When most people think of gut health, probiotics are the first thing that comes to mind. But emerging evidence — particularly from those working at the intersection of neurology, clinical nutrition, and integrative medicine — is showing that gut repair may start with something much more fundamental: cellular fuel.
At the center of this is glutamine, an amino acid that isn’t flashy, trendy, or over-marketed. But it quietly plays a pivotal role in healing a compromised gut lining, supporting immune function, and even regulating how calm or anxious you feel. If you’ve been chasing solutions for bloating, inflammation, or "leaky gut," this might be the most overlooked and effective step you’re not yet taking.
Why the Gut Needs Fuel — And It's Not Just From Food
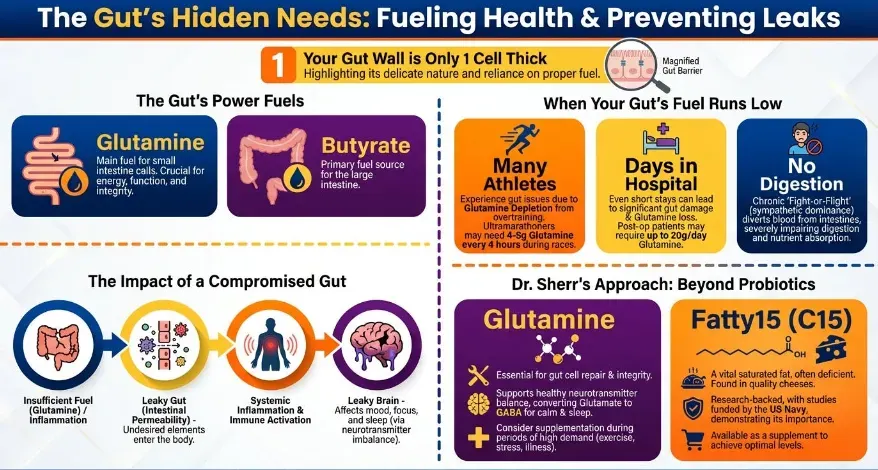
Your gut lining isn’t a passive tube waiting for food to pass through. It's a highly active layer of cells — just one cell thick — that needs fuel to function and protect your body. The small intestine, in particular, relies heavily on glutamine as its primary energy source. Without it, those cells become weak, less effective, and more permeable — what we often refer to as "leaky gut."
Glutamine: The Unsung Hero in Gut Repair and Cellular Energy
Despite its popularity in bodybuilding circles, glutamine isn’t especially useful for muscle growth. But its role in gut lining repair is profound. It fuels the epithelial cells that maintain barrier integrity and prevents tight junctions in the gut from breaking down.
In functional medicine circles, glutamine is increasingly used post-surgery and in hospital settings to preserve gut function and prevent muscle loss. Supplementing with glutamine (typically 4–5g every 4 hours during stress or recovery) has been shown to reduce gut inflammation, protect against immune overactivation, and speed up recovery in endurance athletes and post-op patients alike.
How Leaky Gut Triggers Inflammation, Mood Issues, and Poor Sleep
When the gut becomes permeable, the consequences stretch far beyond digestion. That thin layer of gut lining is your first line of defense between your internal environment and the outside world. Once breached, unwanted molecules — partially digested food, toxins, or pathogens — make their way into the bloodstream, where they can provoke immune system chaos.
This immune response doesn't stay local. It often leads to systemic inflammation and can trigger or worsen everything from food sensitivities to autoimmune conditions. More subtly, many people experience worsened mood, irritability, or fatigue without realizing that gut dysfunction is driving it. And this isn’t just theory — it’s repeatedly observed in clinical practice.
The Gut-Brain Connection: Glutamine, Glutamate, and GABA Explained
Here’s where things get even more interesting. Glutamine doesn't just nourish your gut — it’s also a precursor to neurotransmitters that regulate how you feel. It converts into glutamate, the brain’s main excitatory chemical, and then into GABA, your key calming neurotransmitter.
When Exercise Damages the Gut — And How to Support Recovery
Most people associate exercise with health, and rightly so. But intense or prolonged physical activity — especially endurance events — can deplete glutamine stores rapidly. Endurance athletes often report symptoms like bloating, diarrhea, or abdominal cramping, and in many cases, these are signs of compromised gut function caused by overtraining.
One real-world example? An ultramarathon runner was experiencing severe GI issues during races. With a simple protocol of glutamine supplementation (4–5g every 4 hours) during training and race day, not only did the symptoms vanish, but his performance improved dramatically. His total race time dropped by three hours — without GI distress. It’s a reminder that gut support isn’t optional for high-performance living.
Chronic Stress, Poor Digestion, and Glutamine Depletion
While acute stress from exercise affects gut health physically, chronic emotional stress operates through a different — but equally damaging — mechanism. Stress puts the body in sympathetic (“fight or flight”) mode, diverting blood flow away from the digestive system and impairing enzyme production and nutrient absorption.
This leads to issues like bloating, constipation, SIBO (small intestinal bacterial overgrowth), and nutrient deficiencies. And since stress also depletes magnesium — a cofactor for GABA production — the downstream impact is both gut dysfunction and nervous system imbalance. It’s a loop that feeds itself: stress hurts your gut, and poor gut health amplifies stress.
Why Magnesium and B6 Matter for Gut Health and Sleep
To convert glutamate into calming GABA, your body needs vitamin B6 and magnesium. These aren’t just micronutrients — they’re critical cofactors that make neurotransmitter conversion possible. If you’re low on either (which many people are, especially magnesium), the whole system backs up, leaving you anxious, wired, and unable to relax.
Think of glutamine like the bricks, and B6/magnesium like the mortar holding your neural structure together. Without both, your gut and brain become unstable. Many clinicians now pair glutamine supplementation with magnesium glycinate and activated B6 (P5P) to support better sleep, mood regulation, and gut lining recovery — especially in clients with chronic stress or insomnia.
Real-Life Applications: Glutamine Supplementation That Works
So what does a glutamine protocol look like in practice?- Baseline Support: 5g glutamine 1–2x daily on an empty stomach
- During illness/surgery/post-op: Up to 15–20g/day, split in doses
- Athletic training or endurance events: 5g every 4–6 hours
- Severe gut inflammation: Combined with zinc carnosine, DGL, and mucilaginous herbs
Best taken between meals or before bed, glutamine powder mixes easily into water. For maximum benefit, ensure you’re also supporting cofactors: magnesium (200–400mg) and vitamin B6 (10–50mg P5P form).
Always check with your practitioner — especially if you’re on medications, have neurological conditions, or are working with complex immune challenges.Supporting Gut Repair Beyond Food Alone: What to Expect Over Time
Here’s the honest truth: gut repair isn’t a quick fix. You may feel improvements in days — especially in sleep or bloating — but full restoration often takes months. If you're dealing with long-standing issues like SIBO, post-infectious IBS, or autoimmune flares, expect to layer in dietary support, stress reduction, and possibly targeted antimicrobials or binders.That said, glutamine is one of the few low-risk, high-reward interventions you can begin today. It doesn’t replace probiotics, antimicrobials, or deep functional work — but it lays the foundation. It fuels the cells that protect you. It calms your brain when you can’t think straight. And it works quietly behind the scenes while you do the deeper work of healing.
References
· Rao, R. K., Samak, G., & Rao, V. U. (2012). Role of glutamine in protection of intestinal epithelial tight junctions. Journal of Epithelial Biology & Pharmacology, 5(Suppl 1-M5), 47–54. https://pmc.ncbi.nlm.nih.gov/articles/PMC4369670/
· Cleveland Clinic. (n.d.). Glutamine: Benefits, uses, and risks. Cleveland Clinic. Retrieved January 18, 2026, from https://my.clevelandclinic.org/health/articles/glutamine
· Aydin, O., et al. (2022). Oral glutamine supplementation improves intestinal permeability in diarrhea-predominant irritable bowel syndrome: A randomized controlled trial. Turkish Journal of Gastroenterology, 33(10), 799–806. https://pmc.ncbi.nlm.nih.gov/articles/PMC9549483/
· Rhoads, J. M., et al. (2021). Glutamine and the regulation of intestinal permeability: From bench to bedside. Current Opinion in Clinical Nutrition & Metabolic Care, 24(2), 121–127. https://www.sciencedirect.com/science/article/pii/S2213453021000112
· Wang, B., Wu, G., Zhou, Z., et al. (2017). Glutamine and intestinal barrier function: Molecular mechanisms and clinical applications. Current Opinion in Clinical Nutrition and Metabolic Care, 20(2), 86–91. https://pmc.ncbi.nlm.nih.gov/articles/PMC5454963/