How Alcohol Metabolism Affects Liver Health: Uncovering the Hidden Dangers
Ethanol, commonly found in alcoholic beverages, is metabolized primarily in the liver. While moderate alcohol consumption might be considered safe for some, excessive intake can lead to severe liver damage. This article delves into the intricate process of ethanol metabolism, the toxicity associated with its byproducts, and the variability in how different individuals process alcohol.
The liver's capacity to manage ethanol is a pivotal factor in determining its impact on health. Ethanol metabolism involves several enzymatic pathways that can be influenced by genetic, sex-based, and lifestyle differences. Understanding these pathways is crucial for comprehending how ethanol contributes to liver diseases, both alcoholic and non-alcoholic. Moreover, insights into these processes can aid in developing personalized guidelines for safer alcohol consumption.
The Basics of Ethanol Metabolism
Understanding how ethanol is metabolized in the liver involves a series of biochemical reactions catalyzed by specific enzymes. These reactions can vary based on genetic and environmental factors, influencing how efficiently ethanol is processed and detoxified.
The Role of Alcohol Dehydrogenase
Alcohol dehydrogenase (ADH) is the primary enzyme responsible for metabolizing ethanol. It converts ethanol into acetaldehyde, a toxic intermediate. The efficiency of this enzyme can vary significantly among individuals due to genetic differences. Some people may lack this enzyme entirely, rendering them extremely sensitive to alcohol and often causing them to turn red upon consumption.
- Genetic Polymorphisms: Genetic variations can affect the activity of ADH, influencing how quickly or slowly ethanol is metabolized.
- Sensitivity to Alcohol: Individuals with less active forms of ADH experience heightened sensitivity to alcohol, marked by symptoms such as facial flushing and discomfort.
Acetaldehyde is further metabolized into less harmful substances like carbon dioxide and water. This step is crucial because it prevents the accumulation of toxic intermediates that can cause cellular damage. The entire process involves a delicate balance, and any disruption can lead to harmful effects on the liver.
From Ethanol to Acetaldehyde
The conversion of ethanol to acetaldehyde is a critical step in its metabolism. This process not only involves ADH but also several other enzymes that assist in breaking down acetaldehyde into non-toxic substances. However, the buildup of acetaldehyde, even temporarily, can cause significant harm, attracting inflammatory cells and leading to oxidative stress.
Acetaldehyde's role as a toxic intermediary cannot be overstated. It acts as a magnet for free radicals and other harmful entities, contributing to inflammation and cellular damage. This intermediate stage of ethanol metabolism is where most of the liver damage occurs, making it a focal point for understanding ethanol's impact on liver health.
Toxicity in Ethanol Metabolism
Ethanol metabolism can lead to the production of toxic intermediates, which pose a significant risk to liver health. Understanding the mechanisms of this toxicity is essential for developing effective prevention and treatment strategies.
The Problem with Acetaldehyde
Acetaldehyde is highly toxic and is a primary contributor to the adverse effects of ethanol consumption. Its toxicity arises from its ability to form harmful compounds that can damage cellular structures and functions. Acetaldehyde can attract free radicals, leading to oxidative stress, which further exacerbates liver damage.
- Formation of Harmful Compounds: Acetaldehyde interacts with proteins and DNA, forming adducts that impair cellular functions.
- Oxidative Stress: Free radicals generated by acetaldehyde lead to oxidative damage, a major factor in liver injury.
Inflammatory cells are drawn to areas where acetaldehyde is present, causing a cascade of immune responses that can worsen liver injury. This inflammatory response is a common feature in both alcoholic and non-alcoholic liver diseases, indicating that acetaldehyde's toxicity is a significant factor in liver health.
Inflammatory Response and Liver Damage
The presence of acetaldehyde in the liver triggers an inflammatory response, attracting immune cells that aim to combat the toxin. This influx of immune cells can lead to liver inflammation, contributing to conditions such as hepatitis and cirrhosis. The liver's capacity to manage this inflammation plays a crucial role in determining the extent of damage.
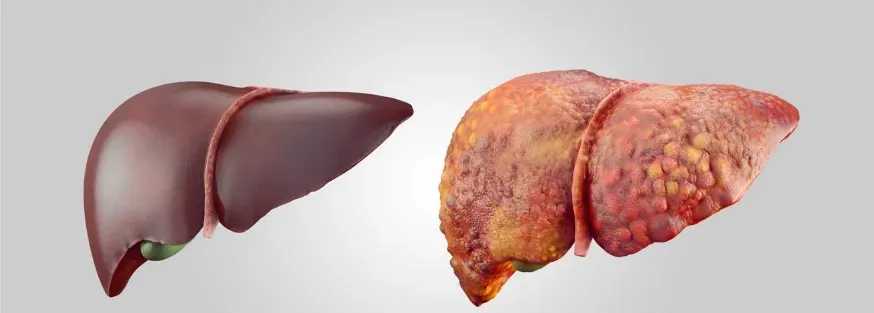
Fat deposition in the liver is another consequence of acetaldehyde toxicity. This altered metabolism at the cellular level can lead to conditions like fatty liver disease. Over time, chronic inflammation and fat accumulation can result in severe liver damage, highlighting the need for understanding and managing ethanol metabolism effectively.
- Conditions Resulting from Inflammation:
- Hepatitis: Inflammation of the liver.
- Cirrhosis: Scarring of the liver tissue.
- Fatty Liver Disease: Accumulation of fat within liver cells.
Understanding these processes can help in the development of strategies to mitigate the harmful effects of ethanol and improve liver health outcomes.
Variability in Ethanol Metabolism
The efficiency of ethanol metabolism varies widely among individuals. This variability can be attributed to genetic, physiological, and environmental factors, all of which play a crucial role in determining an individual's tolerance to alcohol and susceptibility to liver damage.
Genetic Differences in Alcohol Dehydrogenase
Genetic polymorphisms in the alcohol dehydrogenase enzyme can significantly influence how individuals metabolize ethanol. Some people possess variants of this enzyme that are less effective, leading to higher levels of acetaldehyde and increased susceptibility to its toxic effects. These genetic differences are a crucial factor in understanding individual variations in alcohol tolerance and liver health.
- Polymorphisms and Liver Health: Individuals with certain genetic polymorphisms may experience more severe symptoms upon alcohol consumption, including redness and discomfort. These symptoms can serve as indicators of a heightened risk for liver damage, emphasizing the importance of genetic testing and personalized approaches to alcohol consumption.
Sensitivity and Tolerance to Alcohol
Alcohol tolerance varies widely among individuals, influenced by genetic makeup, sex, and other factors. People with lower tolerance levels are more likely to experience adverse effects from even moderate alcohol consumption. This variability underscores the need for personalized guidelines regarding safe alcohol intake.
Tolerance levels can also change over time, influenced by factors like age, body composition, and hormonal changes. Understanding these dynamics is essential for managing alcohol consumption and minimizing the risk of liver damage, particularly in populations with known genetic vulnerabilities.
Factors Influencing Alcohol Tolerance:
- Age: Changes in enzyme activity and liver function over time.
- Body Composition: Differences in muscle and fat distribution.
- Hormonal Changes: Effects of hormonal fluctuations on enzyme activity.
Sex Differences in Ethanol Metabolism
Sex-based differences in ethanol metabolism are significant and have important implications for liver health. These differences arise from variations in body composition, hormonal influences, and genetic factors.
Body Composition and Alcohol Solubility
Sex differences play a significant role in how ethanol is metabolized. Women typically have a higher percentage of body fat compared to men, affecting the solubility and distribution of alcohol in the body. This difference in body composition can influence the severity of ethanol's impact on the liver, with women generally experiencing higher levels of toxicity.
- Fat Solubility: Alcohol is less soluble in fat, leading to higher concentrations in the blood of women compared to men.
- Higher Blood Alcohol Levels: Due to higher fat content, women often have higher blood alcohol concentrations after consuming the same amount of alcohol as men.
The hormonal environment also affects ethanol metabolism, with estrogen and other hormones influencing the efficiency of alcohol dehydrogenase and other enzymes. These factors contribute to the observed differences in alcohol tolerance and liver damage between men and women, necessitating gender-specific guidelines for alcohol consumption.
Pre and Post-Menopausal Differences
The effects of ethanol on the liver can vary significantly between premenopausal and postmenopausal women. Hormonal changes associated with menopause can alter the liver's capacity to metabolize ethanol, potentially increasing susceptibility to its toxic effects. These variations highlight the need for age-specific recommendations for alcohol consumption.
- Premenopausal Women: Higher estrogen levels can affect the activity of enzymes involved in ethanol metabolism, potentially offering some protective effects.
- Postmenopausal Women: The reduction in estrogen levels may lead to decreased enzyme activity and increased vulnerability to liver damage.
Postmenopausal women may experience a reduction in the protective effects of estrogen, leading to increased liver damage from alcohol. Understanding these sex-specific differences is crucial for developing targeted interventions to protect liver health in women across different life stages.
Comparing Alcohol-Related Liver Damage and Metabolic Dysfunction
While alcohol-related liver damage and metabolic dysfunction-associated liver disease share similar features, they differ in their underlying causes. Understanding these similarities and differences is essential for accurate diagnosis and effective treatment.
Similarities in Histological Patterns
Alcohol-related liver damage and metabolic dysfunction-associated liver disease share many histological features. Both conditions involve inflammation, fat deposition, and cellular damage, making it challenging to distinguish between them based on tissue samples alone. These similarities suggest common underlying mechanisms contributing to liver damage.
Histological Features:
- Inflammation: Presence of inflammatory cells in liver tissue.
- Fat Deposition: Accumulation of fat within liver cells.
- Cellular Damage: Structural and functional impairment of liver cells.
The overlapping histological patterns underscore the importance of comprehensive diagnostic approaches that consider patient history, genetic factors, and other variables. Accurate diagnosis is essential for developing effective treatment strategies for both alcoholic and non-alcoholic liver diseases.
Non-Alcoholic vs. Alcoholic Liver Disease
While the histological features of alcoholic and non-alcoholic liver diseases may be similar, their underlying causes and progression can differ. Non-alcoholic liver disease is often associated with metabolic dysfunction, such as obesity and diabetes, while alcoholic liver disease results from excessive alcohol consumption. Despite these differences, both conditions involve similar pathways of inflammation and cellular damage.
Underlying Causes:
- Non-Alcoholic Liver Disease: Linked to obesity, diabetes, and other metabolic disorders.
- Alcoholic Liver Disease: Resulting from chronic excessive alcohol consumption.
Understanding the distinctions and commonalities between these conditions is crucial for developing targeted treatments. Effective management strategies must address the specific factors contributing to liver damage, whether they stem from alcohol consumption or metabolic dysfunction.
Current Research and Unanswered Questions
Ongoing research is essential to uncover the complexities of ethanol metabolism and its effects on liver health. Despite significant progress, many questions remain unanswered, highlighting the need for continued investigation.
The Need for Diverse Cohorts
Current research on ethanol metabolism and liver health highlights the need for studies involving diverse cohorts. Genetic and environmental factors can significantly influence how different populations metabolize ethanol and respond to its toxic effects. Including diverse groups in research is essential for developing comprehensive guidelines and interventions.
Importance of Diversity in Research:
- Genetic Variability: Different populations have unique genetic profiles that affect ethanol metabolism.
- Environmental Influences: Lifestyle and dietary factors can impact liver health and alcohol tolerance.
Understanding the variability in ethanol metabolism across different populations can help identify at-risk individuals and tailor preventive measures accordingly. This approach ensures that recommendations for alcohol consumption are inclusive and effective for all demographic groups.
Future Directions in Alcohol Metabolism Studies
Future research in alcohol metabolism should focus on identifying the precise mechanisms underlying ethanol-induced liver damage. This includes exploring genetic polymorphisms, hormonal influences, and other factors that contribute to individual variability in alcohol tolerance. Advances in molecular biology and genomics hold promise for uncovering these mechanisms.
Key Areas for Future Research:
- Genetic Polymorphisms: Understanding how genetic variations affect enzyme activity and ethanol metabolism.
- Hormonal Influences: Investigating the role of hormones in modulating liver function and ethanol toxicity.
- Personalized Interventions: Developing tailored recommendations and treatments based on individual genetic and environmental factors.
Developing personalized interventions based on genetic and environmental factors is a key goal for future studies. By tailoring recommendations and treatments to individual needs, researchers and healthcare providers can better manage and prevent liver damage associated with alcohol consumption, ultimately improving liver health outcomes for diverse populations.
