Recognizing the Early Signs of Depression: A Comprehensive Guide
Introduction
Depression is a pervasive medical condition impacting millions globally, resonating deeply with diverse individuals and communities. Understanding its breadth and depth is pivotal for anyone interested in maintaining or improving mental health. This overview delves into the essence of depression, discussing not just its clinical aspects but also its profound influence on personal and social levels.
The narrative around depression is often clouded with misconceptions and stigma, making informed awareness and open conversations critical. By examining depression comprehensively, this guide aims to illuminate its early signs, underline the significance of timely intervention, and encourage a proactive stance toward mental wellness. As we explore the nuances of this condition, it's crucial to recognize the varied manifestations of depression that can affect functionality and quality of life across different individuals.
What is Depression?
Depression is more than just fleeting sadness or a temporary feeling of emptiness. It is a diagnosable medical condition characterized by persistent low mood and a severe lack of interest in engaging activities, affecting daily functioning for an extended period. Clinically, it's understood through various symptoms that manifest emotionally, physically, and behaviorally.
Recognizing depression as a complex interplay of neurological, psychological, and socio-environmental factors offers a clearer perspective on its challenges and underscores the necessity for a holistic approach to treatment. This condition demands serious attention and empathy, given its capacity to alter life’s trajectory. Understanding depression's classifications—such as Major Depressive Disorder and Persistent Depressive Disorder—enhances comprehension of its impact and necessary interventions.
Key Early Warning Signs of Depression
Emotional Changes
Among the earliest red flags are profound emotional shifts—persistent sadness, a pervasive sense of hopelessness, or feelings of emptiness that seem to have no end. These are not just bad days; they are consistent feelings that lay heavy on one's spirit, clouding ordinary engagements with a relentless gloom.
Understanding these emotional upheavals is crucial as they are often the first noticeable signs that can alert an individual or their loved ones to the burgeoning grip of depression. Recognizing these signs early can significantly improve the effectiveness of interventions and support systems. Emotional changes often include:
- Persistent melancholy: Not just feeling blue, but a long-lasting sorrow.
- Loss of interest: A significant decrease in interest or pleasure in all or most daily activities.
Physical Symptoms
Depression often manifests silently through physical symptoms that might be overlooked. Common physical signs include unexplained fatigue, disturbances in sleep patterns—either excessive sleep or insomnia—and significant changes in appetite, which can lead to noticeable weight loss or gain.
These physical manifestations are essential indicators because they often present more visibly and can prompt questions about one's health. They serve as critical cues for considering a deeper look into one's mental health status. Key physical symptoms to watch for include:
- Sleep irregularities: Both insomnia and oversleeping.
- Appetite changes: Either a lack of appetite or overeating.
Behavioral Indicators
Behaviorally, depression often leads individuals to withdraw from social activities that they previously enjoyed and to exhibit a general disinterest or inability to engage in personal hobbies or tasks. This withdrawal is not simply a preference for solitude but a more profound detachment from social and recreational engagements.
Noticing these changes in behavior, especially if they represent a significant shift from previous patterns, can be instrumental in identifying the onset of depression. It's often friends or family who first notice these changes, making their role in the supportive network incredibly vital. Common behavioral indicators include:
- Withdrawal from social interactions: Increasing isolation from friends and family.
- Neglecting hobbies and interests: Lack of engagement in previously enjoyed activities.
The Psychological Underpinnings of Depression

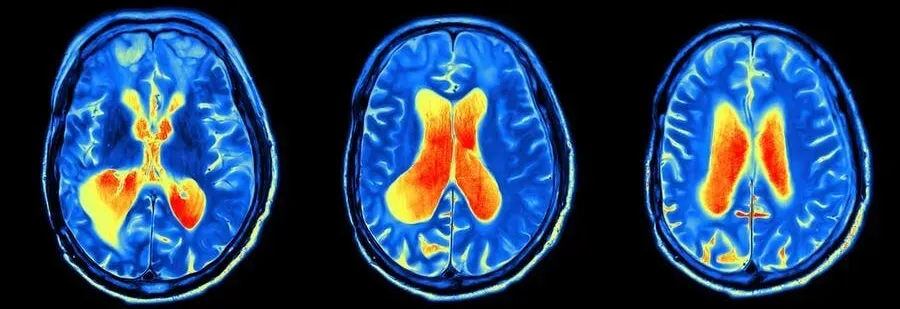
Depression intricately affects thought processes and cognitive functions, leading to challenges in concentration, decision-making, and memory. At its core, it involves a malfunction in the brain's ability to regulate mood and could be linked to an imbalance of neurotransmitters which are critical for communication within the brain.
The psychological landscape of a person with depression is often riddled with intense and persistent negative thinking. This cognitive aspect is crucial for understanding how depression takes hold and dictates behavior, stressing the importance of therapeutic approaches that address these thought patterns. Moreover, understanding the role of neuroplasticity and how depression can alter brain function provides deeper insights into its long-term effects and recovery processes.
Risk Factors for Developing Depression
Genetic Predispositions
Research indicates a significant genetic component to depression, where certain inherited genes can increase the vulnerability to developing depressive disorders. This doesn't guarantee depression but rather highlights a predisposition that might be triggered by various life circumstances.
Awareness and understanding of one's family history regarding mental health can be a crucial step in assessing personal risks and preparing preventive measures or early interventions. Genetic factors typically interplay with environmental triggers to precipitate the onset of depressive episodes.
Environmental Influences
Environmental factors such as prolonged stress, traumatic events, or chronic illness can significantly influence the onset of depression. These conditions create an often overwhelming emotional burden, potentially triggering depression in individuals predisposed by genetic or other factors.
Identifying and modifying these environmental risks where possible can be a strategic part of preventing the onset or exacerbation of depression. Moreover, understanding these influences can foster compassion and support for those struggling within such contexts. Significant environmental influencers include:
- Chronic stress: Ongoing pressures that overwhelm an individual's ability to cope.
- Life events: Major changes or traumatic events such as loss of a loved one or severe financial difficulties.
When to Seek Help

Recognizing the critical stages when professional help becomes necessary is a fundamental aspect of managing depression effectively. If symptoms persist and significantly impair one’s ability to function daily, it is crucial to seek professional advice. Early consultation with healthcare providers can lead to effective management and prevent the condition from worsening.
Moreover, diminishing the stigma associated with seeking help for mental health issues is essential for encouraging more people to step forward. It is a sign of strength, not weakness, to seek help and should be viewed as a proactive measure towards personal health maintenance. It's vital to recognize that help can take various forms, including but not limited to:
- Professional counseling: Engaging with therapists or counselors who specialize in mental health.
- Medical intervention: Consulting with psychiatric professionals for possible medication or other treatments.
Treatment Options and Recovery
Treatment for depression typically includes a combination of psychotherapy, medication, and lifestyle adjustments. Cognitive Behavioral Therapy (CBT) has proven particularly effective in addressing depressive disorders by helping individuals reframe negative thoughts and adopt more constructive behavioral practices.
Furthermore, incorporating routine physical activity, a balanced diet, and sufficient sleep can significantly affect one's mental health and aid in recovery. Personalizing treatment plans to accommodate individual experiences and symptoms is crucial for effective recovery and long-term management of depression. Effective strategies often include:
- Engagement in physical activities: Regular exercise can boost mood and alleviate symptoms of depression.
- Nutritional management: A balanced diet that supports overall brain health and emotional regulation.
Conclusion
Understanding the multi-faceted nature of depression is essential for early recognition, effective treatment, and successful recovery. This guide aims not only to educate but also to empower individuals to take charge of their mental health with proactive strategies and supportive resources.
Remember, seeking support is a courageous step towards recovery, and with the right knowledge and resources, managing and overcoming depression is entirely possible. Let's prioritize mental health with the same rigor we accord physical health, ensuring a balanced approach to overall well-being.



