Do Cell Phones Affect Sperm and Testosterone? What the Science Really Says

Key takeaways
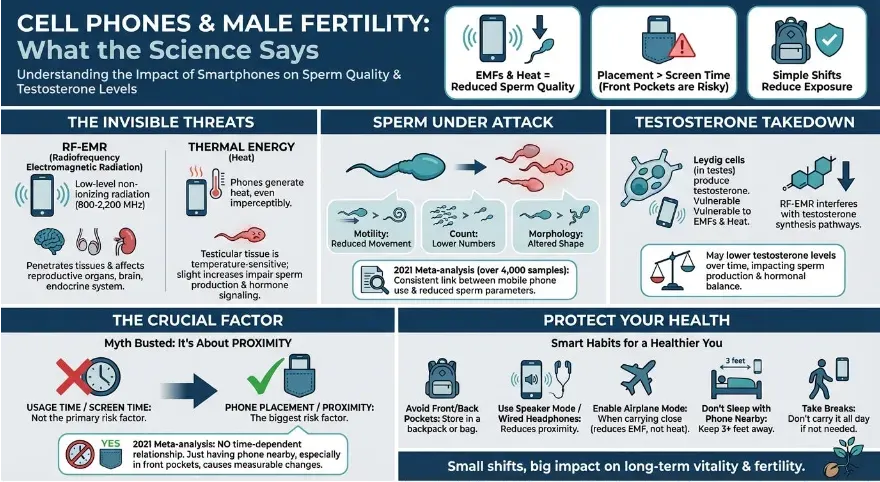
- EMFs and heat from smartphones can reduce sperm quality and may lower testosterone levels.
- Phone placement — not screen time — is the biggest risk factor, especially in front pockets.
- Simple shifts like using a backpack or enabling airplane mode can help reduce exposure.
The culprit? Two main factors: radiofrequency electromagnetic radiation (RF-EMR) and heat. These are emitted by every smartphone — whether it’s in your hand, pocket, or sitting quietly in airplane mode. Let’s break down what the data shows and how you can make smarter choices without going off the grid.
Understanding EMFs, Heat, and Mobile Phone Exposure
Every mobile phone emits RF-EMR — a low-level form of non-ionizing radiation. It’s different from something like X-rays, but that doesn’t mean it’s biologically inert. These frequencies (typically between 800 and 2,200 MHz) penetrate tissues and can affect sensitive systems like the reproductive organs, brain, and endocrine system.
In addition, phones also generate heat — even when you don’t feel it. This matters because testicular tissue is temperature-sensitive. Even slight, sustained increases in temperature around the groin area have been shown to impair sperm production and hormone signaling.
How Phones Impact Sperm Quality: Motility, Count, and Morphology
Sperm are fragile. Their quality — including motility (movement), count, and morphology (shape) — can be impaired by environmental factors. In a 2021 meta-analysis evaluating over 4,000 samples, researchers found a consistent association between mobile phone use and reduced sperm parameters.
Even more surprising: the effect wasn't tied to how long the phone was used. Just having the phone nearby — especially in the pocket — was enough to produce measurable changes. This is likely due to chronic low-level exposure to EMFs and thermal energy near the testicles.
Testosterone Levels and the Role of Leydig Cell Disruption
Testosterone is primarily produced by Leydig cells in the testes. These cells are also vulnerable to environmental stressors, including EMFs and heat. Studies suggest that RF-EMR can interfere with testosterone synthesis pathways, especially intra-testicular testosterone, which is crucial for both sperm production and overall hormonal balance.
The mechanisms aren’t fully mapped yet, but the direction is clear: keeping your phone near your reproductive organs may lower testosterone levels over time, even if you don’t feel immediate symptoms.
Why Phone Placement Matters More Than Screen Time
One of the biggest misconceptions is that it's screen time or usage time that determines the level of risk. Not true. The 2021 meta-analysis emphasized that there’s no time-dependent relationship. It’s not about whether you use your phone for 20 minutes or 4 hours.
What matters most is proximity. Keeping a phone in your front pocket — even for short periods — exposes the testes to low-level radiation and heat consistently throughout the day. The takeaway? Where you keep your phone is more important than how much you use it.
Debunking the "Usage Time" Myth: It's About Exposure, Not Hours
It was once believed that harm from smartphones only occurred after extended usage — like 4+ hours per day. But that’s no longer supported by the data. The most recent studies show that any amount of phone exposure, if it’s near the body, can reduce sperm quality.
Fertility Implications for Men Trying to Conceive
For men actively trying to conceive, small details like phone placement matter. Fertility specialists now often recommend limiting exposure to heat and EMFs as part of preconception care. That includes:
- Avoiding laptops directly on the lap
- Wearing looser underwear
- And yes — keeping phones away from the groin
Can Turning Off Wi-Fi or Bluetooth Reduce the Risk?
Turning off Wi-Fi or cellular data may help reduce RF-EMR exposure, but it doesn't eliminate the risk. Phones still emit some level of EMF even in airplane mode, and the heat factor remains. Many people assume that if the phone isn't actively being used, it’s harmless — but that’s not necessarily true.
To truly minimize exposure, you’d need to physically separate the device from your body — ideally keeping it in a backpack, bag, or on a nearby surface rather than your pocket.
Practical Steps to Minimize Damage While Staying Connected
You don’t have to toss your smartphone to protect your fertility. Here are simple, low-friction ways to minimize the potential downsides:- Avoid front or back pockets: Store your phone in a backpack or bag when possible.
- Use speaker mode or wired headphones: Reduces proximity to sensitive areas like the head or groin.
- Enable airplane mode when carrying close: Especially during workouts or long periods of carrying.
- Don’t sleep with your phone near your body: Keep it across the room or at least 3 feet away.
- Take breaks from having it on your body: Don’t carry it all day if you don’t need to.
Final Thoughts: Small Shifts That May Protect Long-Term Health
Smartphones aren’t going anywhere, but the science is starting to catch up to our usage patterns. While EMF and heat-related risks won’t make headlines like smoking or diet, they represent a modifiable lifestyle factor that directly impacts sperm quality and hormonal health.
For men who are looking to optimize fertility, support testosterone levels, or just take small steps to protect their long-term vitality, the message is clear: keep the phone away from the body whenever possible. It's a low-cost, high-upside adjustment in a world where exposure is nearly impossible to avoid.
